Pain is a universal experience, yet the way individuals perceive and respond to it can vary dramatically. For some, pain serves as a crucial warning signal, alerting them to injury or illness. However, there exists a rare phenomenon known as pain immunity, where certain individuals exhibit an unusual resistance to pain.
This intriguing condition raises questions about the underlying mechanisms that govern pain perception and the genetic factors that contribute to this unique trait. As you delve into the complexities of pain immunity, you will uncover the intricate interplay between genetics and the human experience of pain. Understanding pain immunity not only sheds light on the biological processes involved but also opens up avenues for potential therapeutic interventions.
By exploring the genetic basis of this phenomenon, researchers aim to unravel the mysteries of pain perception and develop innovative treatments for those who suffer from chronic pain conditions. As you navigate through this article, you will gain insights into the genetic disorders associated with pain immunity, their symptoms, and the implications for individuals living with these conditions.
Key Takeaways
- Pain immunity is a rare condition where individuals do not feel physical pain.
- Genetic disorders play a significant role in the development of pain immunity.
- Genetics can influence an individual’s pain perception and tolerance.
- Research is ongoing to explore the genetic basis of pain immunity and related disorders.
- Living with a pain immunity disorder can have significant physical and social implications.
Understanding Genetic Disorders
Genetic disorders arise from abnormalities in an individual’s DNA, which can lead to a wide range of health issues. These disorders can be inherited from one or both parents or may occur spontaneously due to mutations in the genetic material. The complexity of genetic disorders lies in their diverse manifestations, which can affect various systems within the body.
Some genetic disorders are relatively common, while others are exceedingly rare, making them less understood and often overlooked in medical research. As you explore genetic disorders, it becomes evident that they can significantly impact an individual’s quality of life. Some may experience debilitating symptoms that hinder daily activities, while others may have milder manifestations that go unnoticed for years.
The study of genetic disorders is crucial not only for understanding their origins but also for developing effective treatments and interventions. By examining the genetic underpinnings of these conditions, researchers can identify potential therapeutic targets and pave the way for advancements in personalized medicine.
The Role of Genetics in Pain Perception
Genetics plays a pivotal role in how individuals perceive and respond to pain. Variations in specific genes can influence pain sensitivity, tolerance, and even the effectiveness of pain relief medications. For instance, certain genetic polymorphisms have been linked to heightened sensitivity to pain, while others may confer a degree of resistance.
This genetic variability explains why some people seem to endure pain more readily than others and why certain treatments work better for some individuals than for others. As you delve deeper into the genetics of pain perception, you will discover that this field is rapidly evolving. Researchers are employing advanced techniques such as genome-wide association studies (GWAS) to identify specific genes associated with pain sensitivity and immunity.
By understanding these genetic factors, scientists hope to develop targeted therapies that can enhance pain management strategies and improve the overall quality of life for those affected by chronic pain conditions.
Exploring the Genetic Basis of Pain Immunity
| Gene | Function | Impact on Pain Immunity |
|---|---|---|
| SCN9A | Codes for a sodium channel | Associated with congenital insensitivity to pain |
| TRPA1 | Codes for a ion channel | Involved in pain sensation and inflammation |
| COMT | Codes for an enzyme | Regulates pain perception and response to pain |
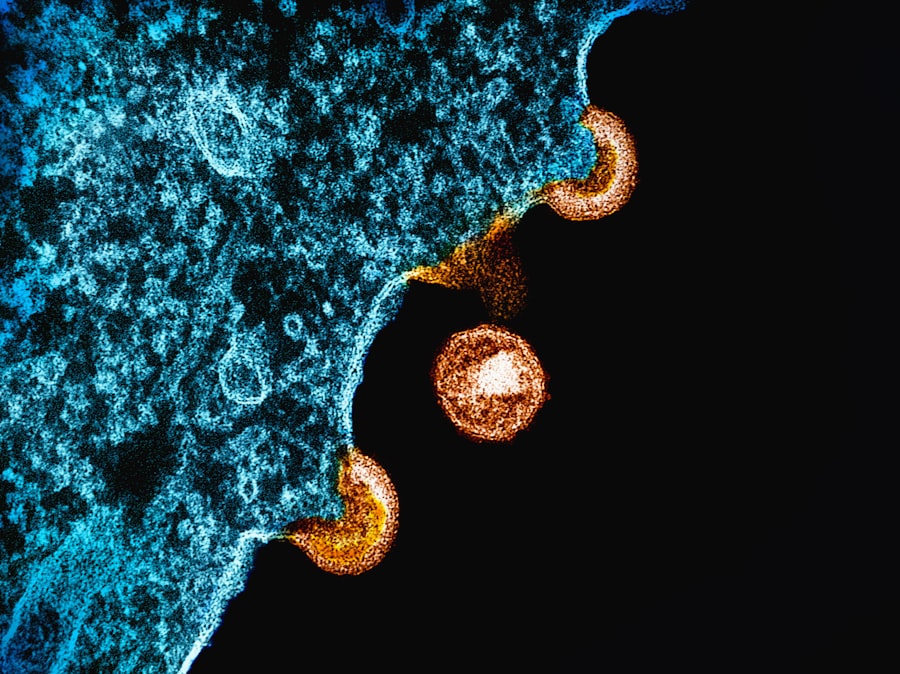
The exploration of pain immunity from a genetic perspective is a fascinating area of research that has garnered significant attention in recent years. Scientists have identified specific genes that appear to play a crucial role in modulating pain perception and response. For example, mutations in genes such as SCN9A have been linked to congenital insensitivity to pain, a rare condition where individuals cannot feel physical pain due to a lack of functional sodium channels involved in transmitting pain signals.
As you consider the implications of these findings, it becomes clear that understanding the genetic basis of pain immunity could revolutionize how we approach pain management. By identifying the molecular pathways involved in pain perception and immunity, researchers can develop novel therapeutic strategies aimed at enhancing or mimicking these protective mechanisms. This could lead to breakthroughs in treating chronic pain conditions that currently lack effective interventions.
Types of Genetic Disorders Related to Pain Immunity
Several genetic disorders are directly associated with pain immunity or altered pain perception. One notable example is congenital insensitivity to pain (CIP), a rare condition characterized by an inability to feel physical pain. Individuals with CIP often face significant challenges due to their inability to recognize injuries or illnesses that would typically elicit a pain response.
This condition highlights the critical role that pain plays in protecting the body from harm. Another disorder worth mentioning is hereditary sensory and autonomic neuropathy (HSAN), which encompasses a group of genetic conditions that affect sensory nerves responsible for transmitting pain signals. Individuals with HSAN may experience diminished or absent sensations of pain, temperature, and touch, leading to an increased risk of injuries and infections.
Understanding these disorders not only provides insight into the mechanisms of pain immunity but also emphasizes the importance of pain as a protective signal in human health.
Symptoms and Effects of Pain Immunity Disorders

Living with a disorder related to pain immunity can present unique challenges and symptoms that differ significantly from typical experiences of pain. Individuals with conditions like congenital insensitivity to pain may not exhibit any physical signs of injury despite suffering from severe trauma or illness. This lack of awareness can lead to serious complications, as they may not seek medical attention until significant damage has occurred.
Moreover, the psychological effects of living without the ability to feel pain can be profound. You may find that individuals with these disorders often grapple with anxiety and fear regarding their health and safety. The absence of pain as a warning signal can create a sense of vulnerability, leading them to constantly assess their surroundings for potential dangers.
Understanding these symptoms is crucial for developing appropriate support systems and interventions for those affected by pain immunity disorders.
Diagnosis and Treatment of Pain Immunity Disorders
Diagnosing genetic disorders related to pain immunity often involves a combination of clinical evaluation, family history assessment, and genetic testing. Healthcare professionals may conduct thorough examinations to identify any physical signs or symptoms associated with these conditions. Genetic testing can provide definitive answers by identifying specific mutations or abnormalities in genes known to be linked to pain perception.
For instance, individuals with congenital insensitivity to pain may require regular monitoring for injuries and proactive measures to prevent complications. Additionally, multidisciplinary approaches involving physical therapy, occupational therapy, and psychological support can help improve overall well-being and quality of life.
Current Research and Advancements in Pain Immunity
The field of pain immunity research is rapidly advancing, driven by technological innovations and a growing understanding of genetics. Researchers are increasingly utilizing cutting-edge techniques such as CRISPR gene editing to explore potential therapeutic interventions for individuals with genetic disorders related to pain perception. By manipulating specific genes associated with pain sensitivity, scientists hope to develop targeted treatments that could enhance or restore normal pain responses.
Moreover, ongoing studies are investigating the role of epigenetics—how environmental factors influence gene expression—in shaping individual responses to pain. This research holds promise for uncovering new pathways involved in pain modulation and could lead to breakthroughs in personalized medicine approaches for managing chronic pain conditions.
Living with a Pain Immunity Disorder
Living with a disorder related to pain immunity presents unique challenges that extend beyond the physical realm. You may find that individuals affected by these conditions often navigate a complex landscape of social interactions and personal relationships. Friends and family members may struggle to understand the implications of living without the ability to feel pain, leading to misunderstandings or misconceptions about the individual’s experiences.
Additionally, individuals with pain immunity disorders may face practical challenges in daily life. Simple activities such as exercising or engaging in physical labor can pose significant risks if one cannot feel discomfort or injury. As such, fostering awareness and understanding within communities is essential for creating supportive environments that accommodate the needs of those living with these conditions.
Ethical and Social Implications of Pain Immunity Disorders
The existence of pain immunity raises important ethical questions regarding medical treatment and societal perceptions of disability. On one hand, individuals who cannot feel physical pain may be viewed as having an extraordinary ability; on the other hand, they face significant risks due to their condition. This duality prompts discussions about how society values different experiences of health and disability.
Furthermore, ethical considerations arise when it comes to research involving genetic manipulation or interventions aimed at altering an individual’s natural state of being. As you reflect on these implications, it becomes clear that ongoing dialogue among researchers, healthcare professionals, ethicists, and affected individuals is essential for navigating the complexities surrounding pain immunity disorders.
Conclusion and Future Directions in Pain Immunity Research
In conclusion, the study of pain immunity offers valuable insights into the intricate relationship between genetics and pain perception. As you have explored throughout this article, understanding the genetic basis of this phenomenon has far-reaching implications for both research and clinical practice. The identification of specific genes associated with altered pain responses opens up new avenues for therapeutic interventions that could transform how we approach chronic pain management.
Looking ahead, continued research into the genetic underpinnings of pain immunity will be crucial for developing targeted treatments and improving outcomes for individuals affected by these rare disorders. As scientists delve deeper into the complexities of genetics and its impact on human health, there is hope for innovative solutions that enhance our understanding of pain perception and ultimately lead to better care for those living with chronic pain conditions.
Recent research has shed light on the fascinating relationship between genetics and pain immunity, particularly in individuals with specific genetic disorders. For a deeper understanding of this topic, you can explore the article on genetic disorders and their implications for pain perception at Freaky Science. This resource provides valuable insights into how certain genetic variations can influence an individual’s ability to experience and manage pain.
WATCH THIS! Why Painlessness Threatens Your Survival
FAQs
What is pain immunity genetic disorder?
Pain immunity genetic disorder is a rare genetic condition that causes individuals to have a reduced ability to feel physical pain.
What causes pain immunity genetic disorder?
Pain immunity genetic disorder is caused by mutations in specific genes that are involved in the transmission of pain signals in the body.
What are the symptoms of pain immunity genetic disorder?
Individuals with pain immunity genetic disorder may experience injuries or illnesses without feeling the usual pain associated with such conditions. They may also have difficulty recognizing when they are injured.
How is pain immunity genetic disorder diagnosed?
Pain immunity genetic disorder can be diagnosed through genetic testing to identify mutations in the specific genes associated with the condition.
Is there a treatment for pain immunity genetic disorder?
Currently, there is no specific treatment for pain immunity genetic disorder. Management typically involves close monitoring for injuries and other health issues, as well as counseling to help individuals understand and cope with their condition.
Is pain immunity genetic disorder hereditary?
Pain immunity genetic disorder is a hereditary condition, meaning it can be passed down from parents to their children through genetic inheritance.
